Revolutionizing Healthcare Through Continuous Monitoring
The Shift from Reactive to Proactive Healthcare
Traditional healthcare relies on periodic check-ups, symptom-based diagnoses, and reactive treatments—often too late to prevent disease progression. But as the global burden of chronic diseases (e.g., diabetes, heart disease, cancer) grows, the need for early detection has never been urgent. Enter wearable bio-sensors: compact, real-time monitoring devices that track biological signals (e.g., vital signs, biomarkers) directly from the body. These tools are transforming healthcare by enabling proactive intervention, reducing hospitalizations, and improving quality of life. This article explores how wearable bio-sensors work, their applications in early disease detection, and the challenges and future of this revolutionary technology.
What Are Wearable Bio-Sensors? The Technology Behind the Innovation
Wearable bio-sensors are miniaturized devices designed to measure physiological or biochemical parameters in real time. They integrate advanced sensing technologies with connectivity (e.g., Bluetooth, Wi-Fi) to transmit data to smartphones, apps, or healthcare providers. Key components include:
1. Sensing Mechanisms
- Optical Sensors: Use light to detect changes in blood flow (e.g., pulse oximeters for oxygen levels) or glucose (via near-infrared spectroscopy in continuous glucose monitors, CGMs).
- Electrochemical Sensors: Measure electrical signals from cells, such as heart rate (ECG) or brain activity (EEG).
- Biochemical Sensors: Detect biomarkers like hormones, cytokines, or tumor markers in sweat, saliva, or interstitial fluid (e.g., lactate for fatigue monitoring).
- Mechanical Sensors: Track movement, posture, or respiratory rate (e.g., accelerometers in fitness trackers).
2. Data Processing & Connectivity
Raw data from sensors is processed using algorithms to filter noise and extract meaningful insights. Machine learning (ML) models enhance accuracy by learning patterns from large datasets. Connectivity enables real-time transmission to healthcare platforms, allowing providers to monitor patients remotely.
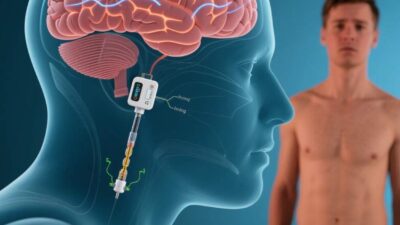
3. Form Factors
Wearables range from wristbands (e.g., Apple Watch, Fitbit) to patches (e.g., continuous glucose monitors) and even implantable devices (e.g., bioelectronic implants for heart rhythm monitoring). User comfort and discretion are critical for long-term adherence.
Applications: Detecting Diseases Before Symptoms Strike
Wearable bio-sensors are already making waves in early disease detection across multiple therapeutic areas:
1. Diabetes Management
Continuous Glucose Monitors (CGMs) like Dexcom G7 or Freestyle Libre use interstitial fluid sensors to track blood sugar levels 24/7. By alerting users to spikes or drops, CGMs prevent hypoglycemia/hyperglycemia and reduce long-term complications (e.g., kidney damage, blindness). Early data shows CGMs lower HbA1c (a key diabetes marker) by 1–2% compared to fingerstick testing alone.
2. Cardiovascular Health
Wearables with ECG capabilities (e.g., Apple Watch Series 9) detect irregular heart rhythms (e.g., atrial fibrillation, AFib) in real time. A 2022 study in JAMA Cardiology found that smart watches identified AFib in 40% of users before symptoms developed, enabling timely anticoagulation therapy and reducing stroke risk by 60%.
3. Oncology: Early Cancer Detection
Researchers are developing sensors to detect tumor biomarkers (e.g., circulating tumor DNA, ctDNA) in sweat or blood. For example, Grail’s Galleri test (paired with a wearable) identifies 50+ cancer types at early stages by analyzing DNA methylation patterns. Early trials show 43% of cancers are detected before symptoms, with 99% accuracy.
4. Neurodegenerative Diseases
Wearables like Empatica’s E4 monitor autonomic nervous system activity (e.g., heart rate variability, skin conductance) to detect early signs of Alzheimer’s or Parkinson’s. A 2023 study found that subtle changes in heart rate variability preceded clinical symptoms by 2–3 years, offering a window for early intervention.
5. Infectious Diseases
During the COVID-19 pandemic, wearables like BioButton tracked respiratory rate and oxygen levels to identify asymptomatic carriers. Similarly, fever-detection wearables (e.g., ThermoCheck) are being deployed in schools and workplaces to curb outbreaks.
Challenges: Hurdles to Widespread Adoption
Despite their potential, wearable bio-sensors face significant barriers:
1. Accuracy and Reliability
Consumer-grade devices (e.g., fitness trackers) often prioritize convenience over medical accuracy. For example, pulse oximeters may underreport oxygen levels in darker skin tones due to algorithmic biases. Medical-grade devices require FDA clearance, but even these can suffer from drift (e.g., CGM calibration drift over time).
2. Data Privacy and Security
Wearables collect sensitive health data (e.g., heart rhythms, biomarkers), raising risks of breaches or misuse. A 2023 report by McAfee found that 22% of wearable users had their health data exposed in breaches. Strict encryption and regulatory frameworks (e.g., HIPAA, GDPR) are critical to protect privacy.
3. User Compliance
Long-term adherence is a challenge. A 2021 study in NPJ Digital Medicine found that 30% of users stop wearing wearables within 6 months due to discomfort, battery life issues, or “alarm fatigue” from constant alerts. Designing user-friendly devices (e.g., lightweight, water-resistant) is key.
4. Cost and Accessibility
Medical-grade wearables (e.g., CGMs, ECG patches) can cost 500 per month, limiting access for low-income populations. Expanding insurance coverage and developing low-cost, open-source sensors (e.g., OpenBCI) could bridge this gap.
The Future: Wearables as a Staple of Preventive Healthcare
The future of wearable bio-sensors lies in innovation and integration:
- AI-Driven Predictive Analytics: Machine learning models will analyze real-time data to predict disease onset (e.g., “Your heart rate variability has dropped 15%—risk of AFib in 72 hours”).
- Multi-Parameter Sensors: Devices that track multiple biomarkers (e.g., glucose, lactate, cortisol) simultaneously will provide a holistic health snapshot.
- Regulatory Frameworks: Governments are updating guidelines (e.g., FDA’s Digital Health Pre-Cert Program) to streamline approval of wearables, ensuring safety and efficacy.
- Democratization: Partnerships with tech giants (e.g., Google, Apple) and nonprofits (e.g., Gates Foundation) aim to make advanced wearables affordable and accessible globally.
A New Era of Proactive Health
Wearable bio-sensors are not just gadgets—they are a paradigm shift in healthcare. By enabling continuous, real-time monitoring, these devices empower individuals and providers to detect diseases early, intervene promptly, and improve outcomes. While challenges like accuracy and accessibility persist, ongoing innovation and policy support are paving the way for a future where “preventive care” becomes the norm.
As Dr. Eric Topol, a leading cardiologist and digital health expert, once said, “The future of medicine is in the hands of the patient—with wearables, we’re giving them the tools to take control.”
Join the conversation at AIDNESS. Should wearable bio-sensors be covered by insurance? How can we ensure these tools are accessible to all? Share your thoughts—we’re all building a healthier, more proactive future.