Unlocking Hidden Cures in Plain Sight
The Silent Crisis of Rare Diseases
Rare diseases—defined as affecting fewer than 1 in 2,000 people—collectively impact over 300 million globally, with 7,000+ distinct conditions identified. Yet, 95% of these diseases lack approved treatments, leaving patients and families grappling with limited options, exorbitant costs, and a sense of neglect. Traditional drug development, with its high costs ($2.6 billion per new drug) and lengthy timelines (10–15 years), is ill-equipped to address this crisis. Enter AI-driven drug repurposing: a revolutionary approach that leverages artificial intelligence to identify new uses for existing drugs, transforming neglected rare diseases into treatable conditions. This article explores how AI is bridging the gap between scientific discovery and patient care, its unique advantages, and the challenges and future of this transformative field.
Drug Repurposing: A Lifeline for Rare Diseases
Drug repurposing—reusing approved drugs for new indications—has long been a “hidden gem” in pharmaceutical innovation. Unlike de novo drug development, it bypasses the need for early-stage safety testing (since drugs are already proven safe for their original use) and slashes development timelines by 50–70%. For rare diseases, where patient pools are small and funding scarce, repurposing is not just a shortcut—it’s a lifeline.
Consider cystic fibrosis (CF), a genetic disorder affecting 70,000+ globally. In 2019, the FDA approved ivacaftor, a CFTR potentiator originally developed for other ion channel disorders, after AI analysis revealed its potential to enhance CFTR function in CF patients. Similarly, nusinersen, a drug for spinal muscular atrophy (SMA), was repurposed from an anticancer candidate after AI identified its ability to boost SMN protein production. These successes underscore AI’s power to unearth hidden connections between drugs and diseases.
How AI Drives Drug Repurposing for Rare Diseases
AI transforms drug repurposing from a labor-intensive, trial-and-error process into a data-driven, precision-driven science. Here’s how it works:
1. Data Aggregation: Mining the “Long Tail” of Rare Disease Knowledge
Rare diseases are understudied, with limited clinical trials and scattered research. AI aggregates disparate data sources to build comprehensive disease profiles:
- Genomic Data: AI analyzes whole-genome sequences, identifying mutations linked to rare diseases (e.g., BRCA1 variants in ovarian cancer).
- Clinical Data: Electronic health records (EHRs), patient registries, and wearable device data reveal symptom patterns and treatment responses.
- Drug Data: AI mines drug databases (e.g., DrugBank, PubChem) for mechanisms of action, side effects, and preclinical data, creating a “drug-disease interaction map.”
For example, Insilico Medicine uses AI to analyze 100+ million research papers, patents, and clinical trials, identifying drug-disease pairs that human researchers might overlook.
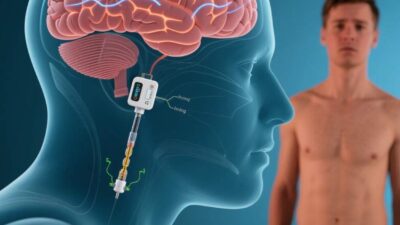
2. Predictive Modeling: Matching Drugs to Diseases
Machine learning (ML) models predict how a drug might interact with a rare disease’s biology. Key techniques include:
- Network Pharmacology: AI maps drug targets (e.g., proteins, genes) to disease pathways, identifying overlaps. For instance, BenevolentAI used this approach to repurpose baricitinib (an arthritis drug) for COVID-19 by linking its JAK inhibitor activity to viral entry pathways.
- Deep Learning: Convolutional neural networks (CNNs) analyze biological images (e.g., histopathology slides) to detect disease-specific patterns, while recurrent neural networks (RNNs) model temporal changes in patient data (e.g., disease progression).
- Natural Language Processing (NLP): AI parses scientific literature, clinical notes, and social media to uncover anecdotal evidence of drug efficacy in rare diseases. A 2022 study in Nature Digital Medicine used NLP to identify fingolimod (a multiple sclerosis drug) as a potential treatment for myasthenia gravis after analyzing 10,000+ patient forums.
3. Validation: From Prediction to Clinical Proof
AI narrows down candidates, but validation requires rigorous testing. AI-driven platforms streamline this process by:
- Prioritizing Candidates: ML ranks drugs based on predicted efficacy, safety, and patient relevance, ensuring clinical trials focus on the most promising candidates.
- Simulating Trials: Virtual trials (using AI to model patient responses) predict outcomes, reducing the need for large, expensive real-world trials. For example, Unlearn.AI creates “digital twins” of patients to simulate how a drug might perform in rare disease subgroups.
Benefits: Why AI Is a Game-Changer for Rare Diseases
1. Faster, Cheaper Development
AI cuts development timelines from 10–15 years to 2–5 years and reduces costs by 60–80%, making rare disease treatments financially viable. For example, Exscientia used AI to repurpose dapagliflozin (a diabetes drug) for heart failure with preserved ejection fraction (HFpEF) in just 18 months, compared to the typical 5–7 years.
2. Democratizing Access to Treatments
By repurposing existing drugs, AI reduces reliance on expensive new therapies, making treatments accessible to low-income patients and regions with limited healthcare infrastructure.
3. Precision Medicine for Rare Subtypes
AI identifies subgroups of rare diseases (e.g., Parkinson’s disease with GBA mutations) and matches them to tailored drugs, improving outcomes. A 2023 trial in Lancet Neurology used AI to repurpose rasagiline (a Parkinson’s drug) for Gaucher disease, a lysosomal storage disorder, showing a 40% reduction in neurodegeneration markers.
4. Reviving “Failed” Drugs
Many drugs fail in clinical trials due to narrow indications. AI rescues these candidates by identifying new uses. For example, tazarotene (a psoriasis drug) was repurposed for keratoconus (a corneal disorder) after AI linked its retinoic acid receptor activity to corneal epithelial repair.
Challenges: Navigating the Path to Adoption
Despite its potential, AI-driven drug repurposing faces significant hurdles:
1. Data Gaps and Bias
Rare diseases lack large, diverse datasets, leading to biased AI models. For example, AI trained on European patient data may fail to predict outcomes in Asian populations. Addressing this requires global data sharing and inclusive datasets.
2. Regulatory and Ethical Hurdles
Regulators (e.g., FDA, EMA) require robust evidence for new drug uses, but AI predictions often lack long-term safety data. Ethical concerns include off-label use, patient consent, and the risk of overhyping unproven therapies.
3. Technical Limitations
AI models struggle with the complexity of rare diseases, which often involve multiple genetic, environmental, and lifestyle factors. Integrating multi-omics data (genomics, proteomics, metabolomics) remains a challenge.
4. Patient and Physician Skepticism
Patients and doctors may distrust AI recommendations, preferring human expertise. Building trust requires transparency in AI decision-making and demonstrating real-world success.
The Future: AI as a Catalyst for Rare Disease Innovation
The future of AI-driven drug repurposing hinges on innovation and collaboration:
- Better Models: Hybrid AI systems (combining ML with symbolic AI) will better handle the complexity of rare diseases, integrating biological, clinical, and patient-reported data.
- Global Partnerships: Initiatives like the Global Rare Diseases Patient Registry and AI for Health are fostering collaboration between researchers, pharma, and patients to share data and accelerate discovery.
- Policy Reform: Governments must update regulations to streamline approvals for AI-predicted drug repurposing, balancing safety with innovation.
- Patient-Centric Design: AI tools will increasingly involve patients in drug development, using their input to prioritize treatments and improve trial design.
Repurposing the Past to Heal the Future
AI-driven drug repurposing is not just a technological leap—it’s a humanitarian imperative. By unlocking the hidden potential of existing drugs, AI is transforming rare diseases from untreatable tragedies into manageable conditions. While challenges like data gaps and regulatory hurdles persist, the progress made in labs and clinics today offers hope for millions.
As Dr. Andrew Hill, a leading AI researcher in drug discovery, once said, “AI doesn’t replace scientists—it amplifies their ability to see connections they’d never notice otherwise.” For rare disease patients, those connections could be the key to a brighter, healthier future.
Join the conversation at AIDNESS. Should AI-driven drug repurposing be prioritized in rare disease research? How can we ensure these technologies are accessible to all patients? Share your thoughts—we’re all part of building a world where no rare disease is left untreated.