Revolutionizing the Fight Against Resistant Infections
The Crisis of Antibiotic Resistance and the Need for Precision
Antibiotic resistance is a global health emergency, with the World Health Organization (WHO) listing it as one of the top 10 threats to humanity. Over 700,000 deaths annually are attributed to drug-resistant infections, and traditional antibiotic therapies—often delivered systemically—fail to target infections precisely, leading to off-target side effects, incomplete eradication, and the acceleration of resistance. Enter microbial nanobots: nanoscale, bio-inspired devices designed to deliver antibiotics directly to infection sites, minimizing collateral damage and maximizing efficacy. By merging nanotechnology with microbial science, these tools are redefining how we combat bacterial infections, offering hope for a post-antibiotic era.
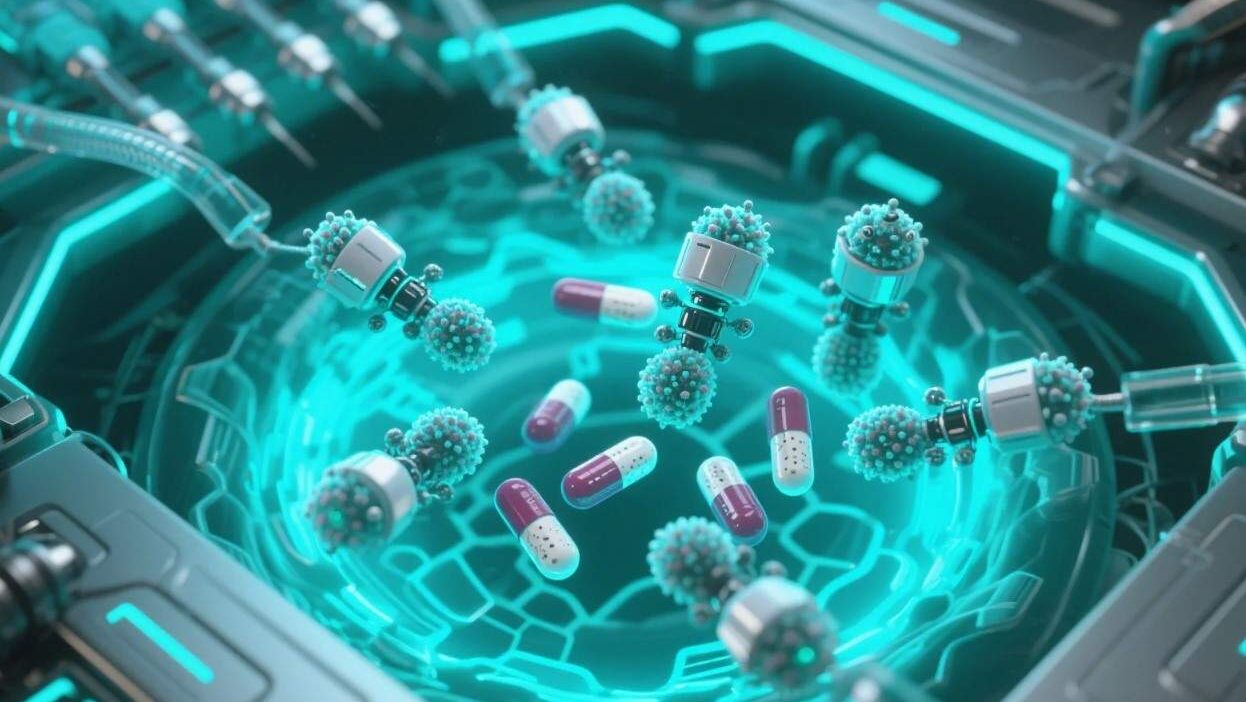
What Are Microbial Nanobots? Design and Function
Microbial nanobots are engineered, nanoscale (1–100 nm) devices that leverage biological components (e.g., proteins, DNA, lipids) or mimic microbial structures to perform targeted tasks. Unlike traditional drug-delivery systems (e.g., liposomes, dendrimers), they are explicitly designed to interact with biological environments, navigate complex tissues, and release antibiotics with spatial and temporal precision.
Key Components
- Structural Scaffold: Made of biocompatible materials like lipid bilayers, poly(lactic-co-glycolic acid) (PLGA), or DNA origami, these scaffolds provide stability and shape.
- Targeting Moieties: Antibodies, peptides, or aptamers (short DNA/RNA sequences) are attached to guide the nanobot to specific pathogens or infected cells (e.g., binding to bacterial cell wall components like peptidoglycan).
- Payload Compartment: Enclosed within the scaffold, this compartment holds antibiotics (e.g., vancomycin, colistin) or antimicrobial agents, protected until release.
- Trigger Mechanisms: Responsive to environmental cues (e.g., pH, enzymes, or oxygen levels) or external signals (e.g., light, magnetic fields), these triggers control drug release at the target site.
How They Work
- Navigation: Guided by targeting moieties, nanobots circulate through the bloodstream or lymphatic system until they bind to infected cells or pathogens.
- Internalization: Some nanobots are taken up by immune cells (e.g., macrophages) that patrol infected tissues, leveraging the body’s natural defense mechanisms.
- Triggered Release: At the target site, environmental triggers (e.g., acidic pH in abscesses, enzymes from immune cells) or external signals (e.g., near-infrared light) prompt the nanobot to release its antibiotic payload.
Applications: Targeting Infections Where They Thrive
Microbial nanobots are being developed for diverse infectious diseases, with early successes in preclinical models:
1. Combating Multidrug-Resistant (MDR) Bacteria
MDR pathogens like Staphylococcus aureus (MRSA) and Pseudomonas aeruginosa are notoriously hard to treat. Nanobots loaded with last-resort antibiotics (e.g., vancomycin, daptomycin) can penetrate biofilms—slimy bacterial colonies that shield pathogens from drugs—and deliver high local concentrations. A 2023 study in Nature Nanotechnology used DNA origami nanobots to deliver vancomycin to MRSA biofilms in mice, reducing bacterial load by 90% compared to free drug.
2. Treating Wound Infections
Chronic wounds (e.g., diabetic ulcers) are prone to persistent infections. Nanobots coated with antimicrobial peptides (AMPs) can target infected wound beds, releasing drugs to kill bacteria while promoting healing. A 2022 trial in Advanced Functional Materials reported that AMP-loaded nanobots accelerated wound closure by 40% in diabetic mice, with minimal scarring.
3. Systemic Infections (e.g., Sepsis)
In sepsis, bacteria spread through the bloodstream, causing organ failure. Nanobots functionalized with opsonins (immune proteins that tag pathogens) can circulate, bind to circulating bacteria, and release antibiotics locally. Early research by MIT’s Institute for Medical Engineering and Science (IMES) demonstrated that such nanobots reduced sepsis mortality in mice by 60%.
4. Intracellular Infections
Some pathogens (e.g., Mycobacterium tuberculosis) hide inside host cells. Nanobots designed to fuse with cell membranes can deliver antibiotics directly into the cytoplasm, bypassing drug efflux pumps. A 2024 preprint in Cell Reports Medicine showed that TB-targeted nanobots eradicated intracellular M. tuberculosis in human macrophages with 95% efficacy.
Benefits: Precision, Efficacy, and Reduced Resistance
Microbial nanobots offer transformative advantages over traditional antibiotic delivery:
- Targeted Delivery: By concentrating antibiotics at infection sites, nanobots reduce systemic exposure, lowering side effects (e.g., kidney damage from vancomycin) and preserving beneficial gut microbiota.
- Overcoming Resistance: High local drug concentrations overwhelm resistant pathogens, even those with efflux pumps or enzyme-mediated drug inactivation.
- Biofilm Penetration: Their small size and bio-inspired surfaces allow nanobots to infiltrate biofilms, a major barrier to conventional antibiotics.
- Multifunctionality: Nanobots can be engineered to deliver multiple drugs (e.g., antibiotics + anti-inflammatory agents) or diagnostic agents (e.g., fluorescent tags to monitor infection clearance), enabling “theranostic” (therapy + diagnosis) applications.
Challenges: Scaling Up and Ensuring Safety
Despite their promise, microbial nanobots face significant hurdles:
1. Manufacturing and Stability
Producing nanobots at scale with consistent quality is challenging. Biological components (e.g., proteins) are prone to degradation, and synthetic materials may trigger immune reactions. Developing scalable, cost-effective fabrication methods (e.g., microfluidic platforms) is critical.
2. Biodistribution and Clearance
Nanobots must navigate the body without being cleared by the liver, spleen, or immune cells. Surface modifications (e.g., PEGylation) can extend circulation time, but long-term safety of these coatings remains unclear.
3. Regulatory and Ethical Hurdles
Regulators (e.g., FDA, EMA) require rigorous safety and efficacy data for novel nanomedicines. Questions about off-target effects, long-term accumulation, and ecological impact (e.g., nanobot shedding into the environment) need addressing.
4. Cost and Accessibility
Early-stage nanobots are expensive to develop, potentially limiting access in low-resource settings. Partnerships with nonprofits and public-private initiatives (e.g., the Bill & Melinda Gates Foundation’s nanomedicine programs) are critical to democratize access.
The Future: Innovation and Impact
The future of microbial nanobots lies in enhancing precision, biocompatibility, and functionality:
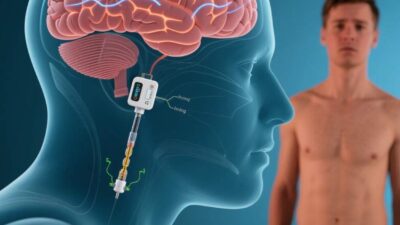
- Smart Nanobots: Integrating AI and biosensors, future nanobots could dynamically adjust drug release based on real-time infection data (e.g., pathogen type, immune response).
- Biodegradable Materials: Using eco-friendly, degradable polymers (e.g., chitosan) or lipid-based systems will reduce long-term toxicity and environmental impact.
- Combination Therapies: Pairing nanobots with immunotherapies (e.g., checkpoint inhibitors) or probiotics could enhance immune responses and prevent recurrence.
- Global Collaboration: Initiatives like the WHO’s Global Action Plan on Antimicrobial Resistance and the EU’s Horizon Europe program are fostering international research to accelerate development.
A New Era of Targeted Antibacterial Warfare
Microbial nanobots are not just a technological leap—they are a strategic response to the antibiotic resistance crisis. By delivering antibiotics with unprecedented precision, these tools offer hope for curing once-incurable infections, reducing healthcare costs, and preserving the efficacy of existing drugs. While challenges like scalability and safety persist, ongoing innovation and collaboration are paving the way for a future where microbial nanobots are a cornerstone of infectious disease treatment.
As nanotechnology expert Dr. Chad Mirkin, director of the International Institute for Nanotechnology, once noted, “Nanobots are the ultimate precision medicine—they let us fight infections where they live, not where they spread.” For patients battling resistant infections, that could mean the difference between life and death.
Join the conversation at AIDNESS. Should microbial nanobots be prioritized in antibiotic research? How can we ensure these technologies are accessible to all? Share your thoughts—we’re all part of building a world where infections are no longer a death sentence.