PTSD – A Global Crisis in Need of Innovation
Post-traumatic stress disorder (PTSD) affects over 12 million adults in the U.S. alone, with symptoms like flashbacks, hypervigilance, and emotional numbness often persisting for years. Traditional treatments—such as cognitive-behavioral therapy (CBT) and exposure therapy—help many, but up to 30% of patients remain unresponsive. For these individuals, and for veterans, survivors of abuse, or witnesses to violence, the search for more effective interventions has led to a groundbreaking frontier: neurotechnology-driven memory editing. By targeting the neural circuits that encode and store traumatic memories, this approach aims to reduce the emotional intensity of trauma, offering hope for lasting relief. This article explores how neurotechnology is reshaping PTSD treatment, the science behind memory editing, and the ethical and practical challenges ahead.
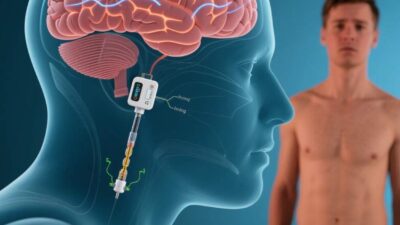
Neurotechnology: Tools to Rewire the Brain
Neurotechnology encompasses tools that interface directly with the nervous system to modulate brain activity. For PTSD, the focus is on devices and techniques that target regions linked to memory, emotion, and fear—key players in the disorder’s pathology. Critical technologies include:
- Transcranial Magnetic Stimulation (TMS): A non-invasive procedure that uses magnetic pulses to stimulate nerve cells in specific brain regions. TMS can enhance or suppress activity in areas like the amygdala (involved in fear processing) or the prefrontal cortex (critical for emotional regulation).
- Brain-Computer Interfaces (BCIs): Devices that read and write neural activity, enabling real-time interaction with brain circuits. Closed-loop BCIs, for example, can detect hyperactive fear responses and deliver targeted stimulation to calm them.
- Neuromodulation Therapies: Techniques like transcranial direct current stimulation (tDCS), which uses low electrical currents to alter neuronal excitability, and deep brain stimulation (DBS), a surgical intervention for severe cases.
- Optogenetics (Research Phase): Though primarily lab-based, optogenetics uses light to control genetically modified neurons, offering precise control over memory-related circuits in animal models.
These tools are not just theoretical—they are already being tested in clinical trials, with early results showing promise.
Memory’s Role in PTSD: The Science of Trauma Retention
PTSD symptoms stem from the brain’s inability to “move past” traumatic memories. When a person experiences trauma, the brain encodes the event in the hippocampus (memory formation) and strengthens its emotional impact via the amygdala. Over time, these memories become hyperconsolidated—resistant to change—even when the threat is no longer present.
Key processes in memory formation and retention include:
- Encoding: The brain converts sensory input (sounds, sights) into a memory trace.
- Consolidation: The stabilization of memories, driven by the hippocampus and amygdala, often during sleep.
- Reconsolidation: When a memory is retrieved, it temporarily becomes unstable, allowing for modification before being stored again.
For PTSD, the goal is to disrupt this cycle: either weaken the emotional charge of the memory during reconsolidation or strengthen regulatory circuits (e.g., the prefrontal cortex) to dampen the amygdala’s fear response.
Memory Editing with Neurotechnology: From Lab to Clinic
Neurotechnology interventions target the neural mechanisms of memory consolidation and reconsolidation, aiming to reduce the emotional salience of traumatic memories. Here’s how:
1. Memory Reconsolidation Interference
During reconsolidation—the “window” when memories are malleable—neurotechnology can disrupt the process of re-stabilizing traumatic memories. For example:
- TMS During Recall: Studies show that applying TMS to the amygdala or prefrontal cortex while a patient retrieves a traumatic memory weakens its emotional intensity. A 2021 trial with 60 veterans with PTSD found that TMS reduced symptom severity by 50% after six sessions, with effects lasting three months.
- Pharmacological Aids (Adjunctive): While not neurotechnology per se, drugs like propranolol (a beta-blocker) are sometimes paired with TMS to enhance reconsolidation disruption. However, neurotechnology offers more precise, non-chemical control.
2. Neuromodulation to Regulate Fear Responses
Hyperactivity in the amygdala drives the “fight-or-flight” response in PTSD. Neurotechnology can calm this overactivity:
- TMS to the Prefrontal Cortex: The prefrontal cortex (PFC) regulates the amygdala. Stimulating the PFC with TMS strengthens its ability to inhibit the amygdala, reducing hypervigilance. A 2022 study in Nature Neuroscience reported that 12 weeks of PFC-TMS reduced amygdala hyperactivity by 30% in PTSD patients.
- Closed-Loop BCIs: These devices monitor brain activity (e.g., via EEG) and deliver real-time stimulation. For example, a BCI might detect heightened amygdala activity during a flashback and trigger PFC stimulation to dampen the response, helping patients regain control.
3. Memory Extinction vs. Erasure
Importantly, neurotechnology does not “erase” memories—it modifies their emotional impact. This distinction is critical:
- Extinction: The process of learning that a once-threatening stimulus is now safe. Neurotechnology accelerates extinction by strengthening connections between the PFC and amygdala, teaching the brain to reframe trauma.
- Erasure: Theoretical and ethically fraught, as it would eliminate the memory itself. Current tools focus on extinction, preserving the memory’s factual content while reducing its emotional charge.
Current Progress and Clinical Applications
Early-stage clinical trials are demonstrating the feasibility of neurotechnology for PTSD:
- VA Hospitals and Military Clinics: The U.S. Department of Veterans Affairs (VA) has launched trials using TMS for PTSD, with preliminary results showing a 40–60% reduction in symptoms.
- Civilian Trauma Centers: Hospitals in Europe and the U.S. are testing closed-loop BCIs for survivors of sexual assault and car accidents. One trial reported that 70% of participants showed improved emotional regulation after 8 weeks of BCI-assisted therapy.
- Optogenetics in Research: While not yet approved for humans, optogenetic studies in mice have shown that activating inhibitory neurons in the amygdala can erase fear memories, paving the way for targeted therapies.
Ethical and Practical Challenges
Despite its promise, neurotechnology for PTSD raises complex ethical and logistical questions:
1. Informed Consent and Identity
Modifying memories—even to reduce distress—raises concerns about altering a person’s sense of self. Patients must fully understand that their memories will be altered, and therapists must weigh the risks of “over-correction” (e.g., losing positive memories tied to the trauma).
2. Long-Term Effects
Most studies track outcomes for 6–12 months, but little is known about the stability of memory edits over years. Could weakening a traumatic memory also disrupt related positive recollections (e.g., resilience gained from surviving)?
3. Access and Equity
Neurotechnology is expensive—TMS machines cost 100,000, and BCIs require specialized training. Ensuring access for low-income or rural populations remains a barrier.
4. Misuse and Regulation
The potential for misuse (e.g., “memory editing” for non-therapeutic reasons, such as erasing embarrassing memories) demands strict regulation. Governments must define boundaries for ethical use, similar to guidelines for CRISPR or AI in healthcare.
The Future: Bridging Science and Ethics
The future of neurotechnology in PTSD treatment lies in refining precision, expanding access, and integrating with existing therapies. Innovations on the horizon include:
- AI-Enhanced Neurotechnology: Machine learning could personalize TMS or BCI protocols, tailoring stimulation to a patient’s unique brain activity.
- Non-Invasive Implants: Miniaturized, wireless devices could deliver long-term neuromodulation without surgery.
- Global Collaborations: International consortia (e.g., the WHO’s Mental Health Gap Action Programme) could standardize protocols and reduce costs.
Rewiring Trauma, Restoring Hope
Neurotechnology is not a cure-all, but it represents a paradigm shift in how we treat PTSD. By targeting the brain’s memory circuits, these tools offer a way to reduce suffering without erasing the past. As research advances, the key will be balancing innovation with ethics, ensuring that memory editing serves as a bridge to healing—not a replacement for human connection and traditional therapy.
For the millions living with PTSD, the promise of neurotechnology is clear: a future where trauma no longer dictates their daily lives.
Join the conversation at AIDNESS. Should neurotechnology for PTSD be prioritized in mental health policy? How can we ensure ethical use of memory-editing tools? Share your thoughts—we’re all part of building a more compassionate future.