The Revolutionary Technology Redefining Drug Development and Medical Research
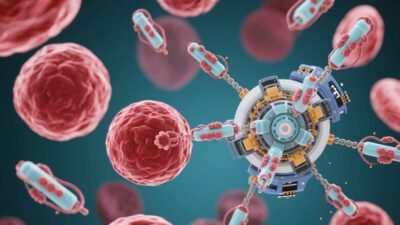
The pharmaceutical industry stands at a crossroads, facing mounting challenges in drug development. Traditional preclinical testing methods using animal models have proven increasingly unreliable, with over 90% of drug candidates failing in human clinical trials despite showing promise in animals. This costly inefficiency – both financially and ethically – has created an urgent need for more accurate human-relevant testing platforms. Organ-on-a-chip (OoC) technology has emerged as a groundbreaking solution, offering miniature, physiologically relevant human organ systems grown from stem cells that can revolutionize how we develop and test new medicines.
The Science Behind Organ-on-a-Chip Technology
Microfluidic Engineering Meets Stem Cell Biology
At the heart of OoC technology lies an elegant convergence of microengineering and regenerative medicine. These thumb-sized devices contain:
- Microfluidic channels (50-300 micrometers wide) that mimic human blood vessels
- Precisely controlled fluid flow (nL to μL per minute) to replicate physiological conditions
- Living human cells arranged in 3D architectures that mimic organ-specific structures
- Integrated sensors for real-time monitoring of physiological parameters
The cells used in these systems are derived from induced pluripotent stem cells (iPSCs) – adult cells reprogrammed to become any cell type needed. This allows researchers to create patient-specific organ models by using an individual’s own cells.
Organ-Specific Implementations
Liver-on-a-Chip: The Detoxification Expert
Liver chips have achieved remarkable progress in replicating human liver functions:
- Sandwich-culture designs with extracellular matrix layers to mimic hepatic architecture
- Oxygen gradients to recreate zonation (periportal vs. perivenous regions)
- Bile canaliculi-like structures for bile acid transport
- Metabolic flux analysis capabilities
Recent breakthroughs include:
- 3D bioprinted liver tissues with functional vascular networks
- Co-cultures with immune cells to study drug-induced liver injury
- Systems incorporating CYP450 enzyme expression monitoring for drug metabolism studies
Lung-on-a-Chip: Breathing New Life into Respiratory Research
Pulmonary chips replicate the lung’s complex mechanical environment:
- Stretchable PDMS membranes (0.2-0.5 Hz frequency) to mimic breathing motions
- Alveolar-capillary barrier reconstruction with tight junctions
- Air-liquid interface cultures for surfactant production
- Mucus production simulation systems
These chips have successfully modeled:
- COVID-19 infection dynamics and antiviral responses
- Acute respiratory distress syndrome (ARDS)
- Drug delivery to deep lung tissues
Heart-on-a-Chip: Beating Heart in a Dish
Cardiac chips focus on replicating heart muscle function with precision:
- Patterned cardiomyocyte monolayers with aligned contractility
- Electrical pacing systems (1-5 Hz) to regulate beating rate
- Calcium imaging capabilities for contraction monitoring
- Mechanical stress application to study hypertrophy
Recent models incorporate:
- Multiple cell types (fibroblasts, endothelial cells) for more realistic tissue
- Drug-induced arrhythmia screening platforms
- Systems for testing gene therapies and electrophysiological interventions
Multi-Organ Systems: Creating Physiologically Relevant Networks
The next frontier in OoC technology involves connecting multiple organ chips to create more comprehensive physiological systems:
Key Technical Considerations
- Standardized fluidic interfaces between chips
- Physiologically-based pharmacokinetic (PBPK) modeling integration
- Automated medium exchange systems
- Real-time data acquisition and analysis platforms
Current Multi-Organ Implementations
- Liver-heart-lung systems for comprehensive drug metabolism studies
- Gut-brain axis models for neuropharmacology research
- Reproductive system chips for endocrine and fertility studies
- Skin-liver systems for dermatological drug testing
Technical Challenges and Limitations
Despite remarkable progress, several challenges remain:
- Vascularization: Creating functional blood vessel networks that can support long-term tissue survival remains a significant hurdle.
- Long-term culture: Most current systems maintain viability for weeks rather than months, limiting their applications.
- Cellular maturity: Many chips use immature cell types that may not fully replicate adult organ functions.
- Standardization: Lack of universal protocols across different research groups hinders reproducibility.
- Scalability: High-throughput screening remains challenging due to the complexity of these systems.
Validation and Regulatory Pathways
For clinical translation, OoC technology must demonstrate:
- Extensive in vitro-in vivo correlation (IVIVC) studies comparing chip results with human clinical data
- FDA and EMA guidance development for OoC-based testing
- Standardized performance metrics and quality control measures
- Comparative studies against gold-standard animal models
- Integration into clinical trial design frameworks
Preliminary studies have shown promising correlations between OoC predictions and human clinical outcomes, particularly in pharmacokinetics and toxicity assessment. Regulatory agencies are actively engaging with researchers to establish validation frameworks.
Economic and Ethical Implications
The potential impact of OoC technology extends beyond scientific advancement:
- Cost reduction: Early estimates suggest 30-50% savings in drug development costs through reduced failure rates.
- Timeline acceleration: Potential to shorten development cycles by 2-3 years.
- Ethical advantages: Complete elimination of animal suffering in drug testing.
- Personalized medicine: Patient-specific drug testing could revolutionize treatment approaches.
- Environmental benefits: Reduced need for animal testing facilities and associated waste.
Future Directions and Emerging Technologies
The field continues to evolve rapidly with several promising developments:
- Organoid-on-a-chip hybrids: Combining stem cell organoids with microfluidic systems for enhanced complexity.
- CRISPR-engineered disease models: Creating chips with specific genetic mutations for precision medicine.
- AI-assisted chip design: Machine learning algorithms to optimize chip architecture and data analysis.
- Wearable OoC systems: Implantable or wearable devices for continuous physiological monitoring.
- Space medicine applications: Studying microgravity effects on human organ function.
A New Era in Drug Development
Organ-on-a-chip technology represents a fundamental shift in how we approach biomedical research and drug development. While challenges remain in perfecting these systems, the progress made to date is undeniable. OoC devices are already providing more accurate human-relevant data than traditional animal models, while offering significant ethical and economic advantages. As the technology matures, we can expect to see:
- Accelerated drug discovery pipelines
- Reduced reliance on animal testing
- More personalized treatment approaches
- Improved success rates in clinical trials
The future of medicine is being written on a chip – and that chip is changing everything.
Key Takeaways
✔ Miniature human organs grown from stem cells on microfluidic chips
✔ More accurate drug testing than animal models
✔ Potential to replace many preclinical animal studies
✔ Significant cost and time savings in drug development
✔ Ethical advantages with no animal testing required
✔ Already in use for COVID-19, cancer, and heart disease research
✔ Future potential for personalized medicine and space applications