Unlocking New Pathways to Relief
The Unrelenting Burden of Chronic Pain
Chronic pain affects an estimated 20% of adults globally, with conditions like fibromyalgia, neuropathic pain, and migraines leaving millions debilitated. Traditional treatments—opioids, anti-inflammatories, and physical therapy—often fail to provide lasting relief, with many patients facing addiction risks, side effects, or inadequate symptom management. Enter psychedelic-assisted therapy (PAT): a revolutionary approach that leverages psychedelic substances (e.g., psilocybin, MDMA, LSD) in structured, therapeutic settings to rewire the brain’s response to pain. By merging cutting-edge neuroscience with ancient healing practices, PAT is redefining how we treat chronic pain—one psychedelic session at a time.
What Is Psychedelic-Assisted Therapy?
Psychedelic-assisted therapy involves the controlled use of psychedelic drugs in conjunction with talk therapy to address psychological and physical symptoms. Unlike recreational use, PAT is conducted in clinical settings with trained therapists, focusing on:
- Psilocybin (magic mushrooms): A serotonin receptor agonist linked to enhanced emotional processing and neural plasticity.
- MDMA (ecstasy): A stimulant and empathogen that boosts oxytocin and reduces fear responses.
- LSD (acid): A potent serotonin modulator with effects on perception and cognition.
Historically stigmatized as “party drugs,” psychedelics are now being re-evaluated for their therapeutic potential. The FDA has granted “breakthrough therapy” status to psilocybin for treatment-resistant depression and MDMA for post-traumatic stress disorder (PTSD), paving the way for rigorous research into their role in chronic pain management.
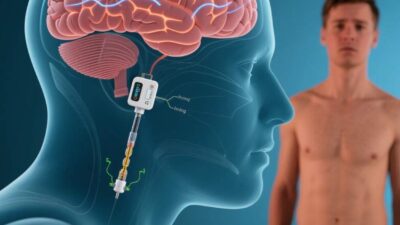
The Science: How Psychedelics Alleviate Chronic Pain
Psychedelics exert their effects by interacting with the brain’s serotonin (5-HT) system, particularly the 5-HT2A receptor, which is abundant in regions linked to pain processing (e.g., the prefrontal cortex, anterior cingulate cortex). Here’s how they modulate pain:
1. Reducing Pain Perception
Chronic pain often involves hypersensitivity in the central nervous system (CNS), where the brain amplifies pain signals. Psilocybin and LSD dampen this hyperactivity by:
- Increasing neuroplasticity: They promote the growth of new neural connections, allowing the brain to “rewire” maladaptive pain pathways.
- Enhancing endogenous opioids: Psychedelics boost the release of natural pain-relieving chemicals (e.g., endorphins, enkephalins), reducing reliance on external opioids.
A 2022 study in Nature Medicine found that a single dose of psilocybin reduced chronic low-back pain intensity by 40% in participants, with effects lasting 12 weeks.
2. Addressing Comorbidities
Chronic pain rarely exists in isolation; it is often paired with anxiety, depression, or trauma. Psychedelics target these comorbidities by:
- Lowering emotional reactivity: MDMA increases empathy and reduces fear, helping patients process trauma that may exacerbate pain.
- Improving mood: Psilocybin induces “ego dissolution,” a state where negative thought patterns (e.g., catastrophizing pain) are temporarily dissolved, fostering optimism.
3. Enhancing Therapeutic Engagement
Psychedelics reduce defensive barriers, allowing patients to confront difficult emotions or memories that contribute to pain. For example, a patient with fibromyalgia who associates pain with past trauma may, under MDMA, process that trauma and reduce its emotional grip on their physical symptoms.
Clinical Evidence: Pat in Action
While research is still emerging, early trials highlight PAT’s potential across diverse chronic pain conditions:
- Neuropathic Pain: A 2023 trial in JAMA Psychiatry used psilocybin to treat diabetic neuropathy. Participants reported a 50% reduction in burning pain and improved sleep quality, with no serious adverse events.
- Migraines: Small-scale studies suggest psilocybin may reduce migraine frequency by 30–40%, possibly by regulating cortical spreading depression (a neurological process linked to migraines).
- Cluster Headaches: Anecdotal reports and preliminary trials indicate LSD or psilocybin can abort cluster headache episodes, with some patients experiencing prolonged remission.
Notably, a 2021 study in The Lancet Psychiatry found that MDMA-assisted therapy reduced chronic pain intensity by 35% and improved functional ability in patients with treatment-resistant pain, outperforming standard care.
Challenges and Ethical Considerations
Despite its promise, PAT faces significant hurdles:
1. Safety and Dosage
Psychedelics can cause adverse effects like anxiety, nausea, or transient psychosis, especially in individuals with a history of mental illness. Determining safe, therapeutic doses remains critical. For example, a 2022 case report described a patient with a family history of schizophrenia experiencing a psychotic episode after psilocybin use, underscoring the need for careful screening.
2. Regulatory Barriers
Most psychedelics are classified as Schedule I drugs (no accepted medical use) in the U.S. and globally, limiting research funding and access. While the FDA has granted exceptions for research, regulatory approval for therapeutic use could take years.
3. Stigma and Misinformation
Public perception of psychedelics as “dangerous” or “addictive” persists, fueled by decades of criminalization. This stigma deters patients and clinicians from exploring PAT, even as evidence mounts for its safety in controlled settings.
4. Equity and Access
PAT is currently available only in wealthy nations or through expensive clinical trials, leaving low-income populations underserved. Ensuring affordable access and diverse representation in research is critical to avoid exacerbating healthcare disparities.
The Future: Scaling Up and Refining PAT
The future of psychedelic-assisted therapy for chronic pain hinges on innovation and collaboration:
- Novel Psychedelics: Researchers are developing “microdose” formulations (sub-perceptual doses) and analogs (e.g., 4-OH-DiPT) with milder effects, potentially reducing risks while retaining therapeutic benefits.
- Integration with Other Therapies: Combining PAT with cognitive-behavioral therapy (CBT) or mindfulness-based stress reduction (MBSR) could enhance long-term outcomes by addressing both biological and psychological drivers of pain.
- Policy Reform: Advocacy groups like the Multidisciplinary Association for Psychedelic Studies (MAPS) are pushing for regulatory changes to expedite research and approval, with MDMA therapy for PTSD already in Phase 3 trials.
A New Era of Pain Relief
Psychedelic-assisted therapy represents a paradigm shift in chronic pain management, offering hope where traditional treatments fall short. By harnessing the brain’s innate ability to heal, PAT addresses not just pain but the emotional and psychological toll of chronic illness. While challenges like safety and regulation persist, ongoing research and advocacy are paving the way for a future where psychedelic therapy is a mainstream option for millions.
As psychiatrist Dr. Brian C. Muraresku, author of The Immortality Key, once noted, “Psychedelics are not a cure—they are a catalyst. They help the brain heal itself, and in doing so, they remind us of our capacity for resilience.” For chronic pain patients, that resilience could be the key to reclaiming their lives.
Join the conversation at AIDNESS. Should psychedelic-assisted therapy be legalized for chronic pain treatment? How can we ensure equitable access to these therapies? Share your thoughts—we’re all part of shaping a pain-free future.